The China Study: Fact or Fallacy?
7072010
Disclaimer: This blog post covers
only a fraction of what’s wrong with “The China Study.” In the years since I
wrote it, I’ve added a number of additional articles expanding
on this critique and covering a great deal of new material. Please read my Forks
Over Knives review for more information on what’s wrong with the conclusions
drawn from Campbell’s casein/aflatoxin research, and if you’d rather look at
peer-reviewed research than the words of some random internet blogger, see my
collection of scientific
papers based on the China Study data that contradict the claims in
Campbell’s book. I’ve also responded
to Campbell’s reply to my critique with a
much longer, more formal analysis than the one on this
page, which you can read
here.
When I first started analyzing the original China
Study data, I had no intention of writing up an actual critique of Campbell’s
much-lauded book. I’m a data junkie. Numbers, along with strawberries and
Audrey Hepburn films, make me a very happy girl. I mainly wanted to see for
myself how closely Campbell’s claims aligned with the data he drew from—if only
to satisfy my own curiosity.
But after spending a solid month and a half reading,
graphing, sticky-noting, and passing out at 3 AM from studious exhaustion upon
my copy of the raw
China Study data, I’ve decided it’s time to voice all my criticisms. And
there are many.
First, let me put out some fires before they have a
chance to ignite:
- I don’t work for the meat or dairy industry. Nor do I have a fat-walleted roommate, best friend, parent, child, love interest, or highly prodigious cat who works for the meat or dairy industry who paid me off to debunk Campbell.
- Due to food sensitivities, I don’t consume dairy myself, nor do I have any personal reason to promote it as a health food.
- I was a vegetarian/vegan for over a decade and have nothing but respect for those who choose a plant-based diet, even though I am no longer vegan. My goal, with the “The China Study” analysis and elsewhere, is to figure out the truth about nutrition and health without the interference of biases and dogma. I have no agenda to promote.
As I mentioned, I’m airing
my criticisms here; this won’t be a China Study love fest, or
even a typical balanced review with pros and cons. Campbell actually raises a
number of points I wholeheartedly agree with—particularly in the “Why Haven’t
You Heard This?” section of his book, where he exposes the reality behind Big
Pharma and the science industry at large. I admire Campbell’s philosophy towards
nutritional research and echo his sentiments about the dangers of scientific
reductionism. However, the internet is already flooded with rave reviews of this
book, and I’m not interested in adding redundant praise. My intent is to
highlight the weaknesses of “The China Study” and the potential errors in
Campbell’s interpretation of the original data.
(IMPORTANT NOTE: My response to Campbell’s reply, as
well as to some common reader questions, can be found in the following post: My
Response to Campbell. Please read this for clarification regarding
univariate correlations and flaws in Campbell’s analytical methods.)
(If this is your first time
here, feel free to browse the earlier posts in the China
Study category to get up to speed.)
On the Cornell University website (the institution
that—along with Oxford University—spawned the China Project), I came across an
excellent summary
of Campbell’s conclusions from the data. Although this article was published
a few years before “The China Study,” it distills some of the book’s points in a
concise, down-n’-dirty way. In this post, I’ll be looking at these statements
along with other overriding claims in “The
China Study” and seeing whether they hold up under scrutiny—including an
in-depth look at Campbell’s discoveries with casein.
(Disclaimer: This post is long. Very long. If either
your time or your attention span is short, you can scroll down to the bottom,
where I summarize the 9,000 words that follow in a less formidable manner.)
(Disclaimer 2: All correlations here are presented as
the original value multiplied by 100 in order to avoid dealing with excessive
decimals. Asterisked correlations indicate statistical significance, with * =
p<0.05, ** = p<0.01, and *** = p<0.001. In other words, the more stars
you see, the more confident we are that the trend is legit. If you’re rusty on
stats, visit the meat
and disease in the China Study page for a basic refresher on some math
terms.)
(Disclaimer 3: The China Study files on the University of Oxford
website include the results of the China Study II, which was conducted after
the first China Study. It includes Taiwan and a number of additional counties on
top of the original 65–and thus, more data points. The numbers I use in this
critique come solely from the first China Study, as recorded in the book “Diet,
Life-style and Mortality in China,” and may be different than the numbers on the
website.)
From Cornell University’s article:
“Even small increases in the
consumption of animal-based foods was associated with increased disease risk,”
Campbell told a symposium at the epidemiology congress, pointing to several
statistically significant correlations from the China studies.
Alright, Mr. Campbell—I’ll hear ya out. Let’s take a
look at these correlations.
Campbell Claim #1
Plasma cholesterol in the
90-170 milligrams per deciliter range is positively associated with most cancer
mortality rates. Plasma cholesterol is positively associated with animal protein
intake and inversely associated with plant protein intake.
No falsification here. Indeed, cholesterol in the
China Project has statistically significant associations with several cancers
(though not with heart disease). And indeed, plasma cholesterol
correlates positively with animal protein consumption and negatively with plant
protein consumption.
But there’s more to the story than that.
Notice Campbell cites a chain of three variables:
Cancer associates with cholesterol, cholesterol associates with animal protein,
and therefore we infer that animal protein associates with cancer. Or from
another angle: Cancer associates with cholesterol, cholesterol negatively
associates with plant protein, and therefore we infer plant protein protects
against cancer.
But when we actually track down the direct
correlation between animal protein and cancer, there is no statistically
significant positive trend. None. Looking directly at animal protein
intake, we have the following correlations with cancers:
Lymphoma: -18
Penis cancer: -16
Rectal cancer: -12
Bladder cancer: -9
Colorectal cancer: -8
Leukemia: -5
Nasopharyngeal: -4
Cervix cancer: -4
Colon cancer: -3
Liver cancer: -3
Oesophageal cancer: +2
Brain cancer: +5
Breast cancer: +12
Penis cancer: -16
Rectal cancer: -12
Bladder cancer: -9
Colorectal cancer: -8
Leukemia: -5
Nasopharyngeal: -4
Cervix cancer: -4
Colon cancer: -3
Liver cancer: -3
Oesophageal cancer: +2
Brain cancer: +5
Breast cancer: +12
Most are negative, but none even reach statistical
significance. In other words, the only way Campbell could indict animal protein
is by throwing a third variable—cholesterol—into the mix. If animal protein were
the real cause of these diseases, Campbell should be able to cite a direct
correlation between cancer and animal protein consumption, which would show that
people eating more animal protein did in fact get more cancer.
But what about plant protein? Since plant protein
correlates negatively with plasma cholesterol, does that mean plant protein
correlates with lower cancer risk? Let’s take a look at the cancer correlations
with “plant protein intake”:
Nasopharyngeal cancer:
-40**
Brain cancer: -15
Liver cancer: -14
Penis cancer: -4
Lymphoma: -4
Bladder cancer: -3
Breast cancer: +1
Stomach cancer: +10
Rectal cancer: +12
Cervix cancer: +12
Colon cancer: +13
Leukemia: +15
Oesophageal cancer +18
Colorectal cancer: +19
Brain cancer: -15
Liver cancer: -14
Penis cancer: -4
Lymphoma: -4
Bladder cancer: -3
Breast cancer: +1
Stomach cancer: +10
Rectal cancer: +12
Cervix cancer: +12
Colon cancer: +13
Leukemia: +15
Oesophageal cancer +18
Colorectal cancer: +19
We have one statistically significant correlation
with a rare cancer not linked to diet (nasopharyngeal cancer), but we also have
more positive correlations than we saw with animal protein.
In fact, when we look solely at the variable “death
from all cancers,” the association with plant protein is +12. With animal
protein, it’s only +3. So why is Campbell linking animal protein to cancer, yet
implying plant protein is protective against it?
In addition, Campbell’s statement about cholesterol
and cancer leaves out a few significant points. What he doesn’t mention is that
plasma cholesterol is also associated with several non-nutritional variables
known to raise cancer risk—namely schistosomiasis infection (correlation of
+34*) and hepatitis B infection (correlation of +30*).
Not coincidentally, cholesterol’s strongest cancer
links are with liver cancer, rectal cancer, colon cancer, and the sum of all
colorectal cancers. As we saw in the posts onmeat
consumption and fish
consumption, schistosomiasis and hepatitis B are the two biggest factors in
the occurrence of these diseases. So is it higher cholesterol (by way of animal
products) that causes these cancers, or is it a misleading association because
areas with high cholesterol are riddled with other cancer risk factors? We can’t
know for sure, but it does seem odd that Campbell never points out the latter
scenario as a possibility.
Campbell Claim #2
Breast cancer is associated
with dietary fat (which is associated with animal protein intake) and inversely
with age at menarche (women who reach puberty at younger ages have a greater
risk of breast cancer).
Campbell is correct that breast cancer negatively
relates to the age of first menstruation—a correlation of -20. Not statistically
significant, but given what we know about hormone exposure and breast cancer, it
certainly makes sense. And there is a correlation between fat intake
and breast cancer—a non-statistically-significant +18 for fat as a percentage of
total calories and +22 for total lipid intake. But are there any dietary or
lifestyle factors with a similar or stronger association than this? Let’s look
at the correlation between breast cancer and a few other variables. Asterisked
items are statistically significant:
Blood glucose level:
+36**
Wine intake: +33*
Alcohol intake: +31*
Yearly fruit consumption: +25
Percentage of population working in industry: +24
Hexachlorocyclohexane in food: +24
Processed starch and sugar intake: +20
Corn intake: +20
Daily beer intake: +19
Legume intake: +17
Wine intake: +33*
Alcohol intake: +31*
Yearly fruit consumption: +25
Percentage of population working in industry: +24
Hexachlorocyclohexane in food: +24
Processed starch and sugar intake: +20
Corn intake: +20
Daily beer intake: +19
Legume intake: +17
Looks to me like breast cancer may have links with
sugar and alcohol, and perhaps also with hexachlorocyclohexane and occupational
hazards associated with industry work. Again, why is Campbell singling out fat
from animal products when other—stronger—correlations are present?
Certainly, consuming dairy and meat from
hormone-injected livestock may logically raise breast cancer risk due to
increased exposure to hormones, but this isn’t grounds for generalizing all
animal products as causative for this disease. Nor is a correlation of +18 for
fat calories grounds for indicting fat as a breast cancer risk factor, when
alcohol, processed sugar, and starch correlate even more strongly. (Animal
protein itself, for the record, correlates with breast cancer at +12—which is
lower than breast cancer’s correlation with light-colored vegetables, legume
intake, fruit, and a number of other purportedly healthy plant foods.)
Campbell Claim #3
For those at risk for liver
cancer (for example, because of chronic infection with hepatitis B virus)
increasing intakes of animal-based foods and/or increasing concentrations of
plasma cholesterol are associated with a higher disease risk.
Ah, here’s one that may be interesting! Even if
animal products don’t cause cancer, do they spur its occurrence when other risk
factors are present? That would certainly be in line with Campbell’s research on
aflatoxin and rats, where the milk protein casein dramatically increased cancer
rates.
So, let’s look only at the counties with the highest
rates of hepatitis B infection and see what animal food consumption does there.
In the China Study, one documented variable is the percentage of each county’s
population testing positive for the hepatitis B surface antigen. Population
averages ranged from 1% to 29%, with a mean of 13% and median of 14%. If we take
only the counties that have, say, 18% or more testing positive, that leaves us
with a solid pool of high-risk data points to look at.
Animal product consumption in these places ranges
from a meager 6.9 grams per day to a heftier 148.1 grams per day—a wide enough
range to give us a good variety of data points. Liver cancer mortality ranges
from 5.51 to 59.63 people per thousand.
Let’s crunch these numbers, shall we? Here’s a chart
of the data I’m using.
When we map out liver cancer mortality and animal
product consumption only in areas with high rates of hepatitis B infection (18%
and higher), we should see cancer rates rise as animal product
consumption increases—at least, according to Campbell. That would indicate
animal-based foods do encourage cancer growth. But here’s what we really
get.
In these high-risk areas for liver cancer, total
animal food intake has a correlation with liver cancer of… dun dun dun… +1.
That’s it. One. We rarely get a perfect statistical
zero in the real world, but this is pretty doggone close to neutral. Broken up
into different types of animal food rather than total consumption, we have the
following correlations:
- Meat correlates at -7 with liver cancer in high-risk counties
- Fish correlates at +11
- Eggs correlate at -29
- Dairy correlates at -19
In other words, it looks like animal foods have
virtually no effect—whether positive or negative—on the occurrence of liver
cancer in hepatitis-B infected areas.
Campbell mentioned plasma cholesterol also associates
with liver cancer, which is correct: The raw correlation is a statistically
significant +37. If it’s true blood cholesterol is somehow an instigator for
liver cancer in hepatitis-B-riddled populations, we’d expect to see this
correlation preserved or heightened among our highest-risk counties. So let’s
take a look at the same previous 19 counties with high hepatitis B occurrence,
and graph their total cholesterol alongside their liver cancer rates.
In the high-risk groups, the correlation between
total cholesterol and liver cancer drops from +37 to +8. Still slightly
positive, but not exactly damning.
If I were Campbell, I’d look at not only animal
protein and cholesterol in relation to liver cancer, but also at the many other
variables that correlate positively with the disease. For instance, daily liquor
intake correlates at +33*, total alcohol intake correlates at +28*, cigarette
use correlates at +27*, intake of the heavy metal cadmium correlates at +38**,
rapeseed oil intake correlates at +25*—so on and so forth. All are statistically
significant. Why doesn’t Campbell mention these factors as possible causes of
increased liver cancer in high-risk areas? And, more importantly, why doesn’t
Campbell account for the fact that many of these variables occur alongside
increased cholesterol and animal product consumption, making it unclear what’s
causing what?
Campbell Claim #4
Cardiovascular diseases are
associated with lower intakes of green vegetables and higher concentrations of
apo-B (a form of so-called bad blood cholesterol) which is associated with
increasing intakes of animal protein and decreasing intakes of plant
protein.
Alright, we’ve got a multi-parter here. First, let’s
see what the actual correlations are between cardiovascular diseases and green
vegetables—an interesting connection, if it holds true. The China Study
accounted for this variable in two ways: one through a diet survey that measured
how many grams of green vegetables each county averaged per day, and one through
a questionnaire that recorded how many times per year citizens ate green
vegetables.
From the diet survey, green vegetable intake (average
grams per day) has the following correlations:
Myocardial infarction and
coronary heart disease: +5
Hypertensive heart disease: -4
Stroke: -8
Hypertensive heart disease: -4
Stroke: -8
From the questionnaire, green vegetable intake (times
eaten per year) has the following correlations:
Myocardial infarction and
coronary heart disease: -43**
Hypertensive heart disease: -36*
Stroke: -35*
Hypertensive heart disease: -36*
Stroke: -35*
A little odd, oui? When we look at total
quantity of green vegetables consumed (in terms of weight), we’ve got only
weak negative associations for two cardiovascular conditions, and a slightly
positive association for heart attacks (myocardial infarction) and coronary
heart disease. Nothing to write home about. But when we look at the number
of times per year green vegetables are consumed, we have much stronger
inverse associations with all cardiovascular diseases. Why the huge difference?
Why would frequency be more protective than quantity? What accounts for this
mystery?
It could be that the China Study diet survey did a
poor job of tracking and estimating greens intake on a long-term basis (indeed,
it was only a three-day survey, although when repeated at a later date yielded
similar results for each county). But the explanation could also boil down to
one word: geography.
Let me explain.
The counties in China that eat greens year-round live
in a particular climate and latitude—namely, humid regions to the south. The
“Green vegetable intake, times per year” variable has a correlation of -68***
with aridity (indicating a humid climate) and a correlation of -60*** with
latitude (indicating southerly placement on the ol’ map). Folks living in these
regions might not eat the most green vegetables quantity-wise, but they do eat
them frequently, since their growing season is nearly year-round.
In contrast, the variable “Green vegetable intake,
grams per day” has a correlation of only -16 with aridity and +5 with latitude,
indicating much looser associations with southern geography. The folks who eat
lots of green veggies don’t necessarily live in climates with a year-round
growing season, but when green vegetables are available, they eat a lot
of them. That bumps up the average intake per day, even if they endure some
periods where greens aren’t on the menu at all.
If green vegetables themselves were protective of
heart disease, as Campbell seems to be implying, we would expect their
anti-heart-disease effects to be present in both quantity of consumption and
frequency of consumption. Yet the counties eating the most greens quantity-wise
didn’t have any less cardiovascular disease than average. This tells us there’s
probably another variable unique to the southern, humid regions in China that
confers heart disease protection—but green veggies aren’t it.
Some of the hallmark variables of humid southern
regions include high fish intake, low use of salt, high rice consumption (and
low consumption of all other grains, especially wheat), higher meat consumption,
and smaller body size (shorter height and lower weight). And as you’ll see in an
upcoming post on heart disease, these southerly regions also had more intense
sunlight exposure and thus more vitamin D—an important player in heart disease
prevention.
(And for the record, as a green-veggie lover myself,
I’m not trying to negate their health benefits—promise! I just want to offer
equal skepticism to all claims, even the ones I’d prefer to be true.)
Basically, Campbell’s implication that green
vegetables are associated with less cardiovascular disease is misleading. More
accurately, certain geographical regions have strong correlations with
cardiovascular disease (or lack thereof), and year-round green vegetable
consumption is simply an indicator of geography. Since only frequency and not
actual quantity of greens seems protective of heart disease and stroke, it’s
safe to say that greens probably aren’t the true protective factor.
So that about covers it for greens. What about the
next variable in Campbell’s claim: a “bad” form of cholesterol called apo-B?
Campbell is justified in noting the link
between apolipoprotein B (apo-B) and cardiovascular disease in the China Study
data, a connection widely recognized by the medical community today. These are
its correlations with cardiovascular disease:
Myocardial infarction and
coronary heart disease: +37**
Hypertensive heart disease: +35*
Stroke: +35*
Hypertensive heart disease: +35*
Stroke: +35*
And he’s also right about the negative association
between apo-B and plant protein, which is -37*, as well as the positive
association between apo-B and animal protein, which is +25* for non-fish protein
and +16 for fish protein. So from a technical standpoint, Campbell’s statement
(aside from the green veggie issue) is legit.
However, it’s the implications of this claim that are
misleading. From what Campbell asserts, it would seem that animal products are
ultimately linked to cardiovascular diseases and plant protein is ultimately
protective of those diseases, and apo-B is merely a secondary indicator of this
reality. But does that claim hold water? Here’s the raw data.
Correlations between animal protein and
cardiovascular disease:
Myocardial infarction and
coronary heart disease: +1
Hypertensive heart disease: +25
Stroke: +5
Hypertensive heart disease: +25
Stroke: +5
Correlations between fish protein and
cardiovascular disease:
Myocardial infarction and
coronary heart disease: -11
Hypertensive heart disease: -9
Stroke: -11
Hypertensive heart disease: -9
Stroke: -11
Correlations between plant protein and
cardiovascular disease (from the China Study’s “diet survey”):
Myocardial infarction and
coronary heart disease: +25
Hypertensive heart disease: -10
Stroke: -3
Hypertensive heart disease: -10
Stroke: -3
Correlations between plant protein and
cardiovascular disease (from the China Study’s “food composite
analysis”):
Myocardial infarction and
coronary heart disease: +21
Hypertensive heart disease: 0
Stroke: +12
Hypertensive heart disease: 0
Stroke: +12
Check that out! Fish protein looks weakly protective
all-around; non-fish animal protein is neutral for coronary heart disease/heart
attacks and stroke but associates positively with hypertensive heart disease
(related to high blood pressure); and plant protein actually correlates fairly
strongly with heart attacks and coronary heart disease. (The China Study
documented two variables related to plant protein: one from a lab analysis of
foods eaten in each county, and one from a diet survey given to county
citizens.) Surely, there is no wide division here between the protective or
disease-causing effects of animal-based protein versus plant protein. If
anything, fish protein looks the most protective of the bunch. No wonder
Campbell had to cite a third variable in order to vilify animal products and
praise plant protein: Examined directly, they’re nearly neck-and-neck.
If you’re wondering about the connection between
animal protein and hypertensive heart disease, by the way, it’s actually hiked
up solely by the dairy variable. Here are the individual correlations between
specific animal foods and hypertensive heart disease:
Milk and dairy products intake:
+30**
Egg intake: -28
Meat intake: -4
Fish intake: -14
Egg intake: -28
Meat intake: -4
Fish intake: -14
You can read more about the
connection between dairy and hypertensive heart disease in the entry on dairy
in the China Study.
At any rate, Campbell accurately
points out that apo-B correlates positively with cardiovascular diseases. But to
imply animal protein is causative of these diseases—and green vegetables or
plant protein protective of them—is dubious at best. What factors cause both
apo-B and cardiovascular disease risk to increase hand-in-hand? This is
the question we should be asking.
Campbell Claim
#5
Colorectal
cancers are consistently inversely associated with intakes of 14 different
dietary fiber fractions (although only one is statistically significant).
Stomach cancer is inversely associated with green vegetable intake and plasma
concentrations of beta-carotene and vitamin C obtained only from plant-based
foods.
This is congruous with conventional
beliefs about fiber being helpful for colon health. And as a plant-nosher
myself, I hope it’s true—but that’s no reason to omit this claim from critical
examination. Here are all of the China Study’s fiber variables as they correlate
to colorectal cancer:
Total fiber
intake: -3
Total neutral detergent fiber intake: -13
Hemi-cellulose fiber intake: -10
Cellulose fiber intake: -13
Intake of lignins remaining after cutin removed: -9
Cutin intake: -14
Starch intake: -1
Pectin intake: +3
Rhamnose intake: -26*
Fucose intake: +2
Arabinose intake: -18
Xylose intake: -15
Mannose intake: -13
Galactose intake: -24
Total neutral detergent fiber intake: -13
Hemi-cellulose fiber intake: -10
Cellulose fiber intake: -13
Intake of lignins remaining after cutin removed: -9
Cutin intake: -14
Starch intake: -1
Pectin intake: +3
Rhamnose intake: -26*
Fucose intake: +2
Arabinose intake: -18
Xylose intake: -15
Mannose intake: -13
Galactose intake: -24
Surprise, surprise: I agree with
Campbell on this one! All but two of the fiber variables have inverse
associations with colorectal cancers. The first part of Campbell Claim #5 passes
Denise’s BS-o-Meter test. Let us celebrate!
…But before we get too jiggy with
it, I do have a nit to pick. Fiber intake also negatively correlates with
schistosomiasis infection, a type of parasite. Try Googling “schistosomiasis
and colorectal cancer” and you’ll get more relevant hits than you’ll ever
have time to read. I’ll elaborate on this in a few paragraphs, so hang tight—but
for now, I’ll just point out two things:
- Schistosomiasis infection is a very strong predictor for colon and rectal cancers, more so than any of the other hundreds of variables studied in the China Project (it has a correlation of +89 with colorectal cancer).
- The only fiber factions that don’t appear protective of colorectal cancer (pectin and fucose) also have the most neutral associations with schistosomiasis infection (+1 and -5, respectively—whereas other fiber factions had correlations ranging from -9 to -27 with schistosomiasis). In all cases, the correlation between each fiber faction and colorectal cancer parallels its correlation with schistosomiasis.
In other words: Is it the fiber
itself that’s protective against colorectal cancer, or is it the fact that the
counties eating the most fiber happened to also have the lowest rates of
schistosomiasis? It would, I think, be wise to prune these variables apart
before declaring fiber itself as protective based on the China Study data.
There is research
conducted outside of the China Project suggesting fiber benefits colon health,
but often that association dissolves when researchers adjust for other dietary
risk factors, such as with the this pooled analysis of
colorectal cancer studies published in the Journal of the American Medical
Association. Bottom line: It’s never a good idea to go looking for a specific
trend just because we believe it should be there. Chains of confirmation bias
are often what cause nutritional myths to emerge and persist. Fiber may be
beneficial, but we shouldn’t approach the data already expecting to find
this—lest we overlook other important influences.

Moving on. Now, what about the
second part of this claim: Stomach cancer is inversely associated with green
vegetable intake and plasma concentrations of beta-carotene and vitamin C
obtained only from plant-based foods.
Is this a fair assessment?
Let’s find out. Here are the correlations between stomach cancer and each of
these variables.
Green
vegetables, daily intake: +5
Green vegetables, times eaten per year: -35**
Plasma beta-carotene: -14
Plasma vitamin C: -13
Green vegetables, times eaten per year: -35**
Plasma beta-carotene: -14
Plasma vitamin C: -13
Ah, looks like we’re facing the Green Veggie Paradox
once again. The folks with year-round access to green vegetables get less
stomach cancer, but the the folks who eat more green vegetables overall aren’t
protected. Once again, I’ll suggest that a geographic variable specific to
veggie-growing regions could be at play here.
As for beta-carotene and vitamin C concentrations in
the blood, Campbell is correct in noting an inverse association with stomach
cancer. However, the correlations aren’t statistically significant, nor are they
very high: -14 and -13, respectively.
Campbell Claim #6
Western-type
diseases, in the aggregate, are highly significantly correlated with increasing
concentrations of plasma cholesterol, which are associated in turn with
increasing intakes of animal-based foods.
From his book, we know Campbell defines Western-type
diseases as including heart disease, diabetes, colorectal cancers, breast
cancer, stomach cancer, leukemia, and liver cancer. And indeed, the variable
“total cholesterol” correlates positively with many of these diseases:
Myocardial infarction and
coronary heart disease: +4
Diabetes: +8
Colon cancer: +44**
Rectal cancer: +30*
Colorectal cancer: +33**
Breast cancer: +19
Stomach cancer: +17
Leukemia: +26*
Liver cancer: +37*
Diabetes: +8
Colon cancer: +44**
Rectal cancer: +30*
Colorectal cancer: +33**
Breast cancer: +19
Stomach cancer: +17
Leukemia: +26*
Liver cancer: +37*
Perhaps surprisingly, total cholesterol has only weak
associations with heart disease and diabetes—weaker, in fact, than the
correlation between these conditions and plant protein intake (+25 and +12,
respectively). But we’ll put that last point aside for the time being. For now,
let’s focus on the diseases with statistical significance, which include all
forms of colorectal cancer, leukemia, and liver cancer. (Despite classifying
stomach cancer as a “Western disease,” by the way, China actually has far higher
rates of this disease than any Western nation. In fact, half the
people who die each year from stomach cancer live in China.)
First, let’s dive into the dark, murky chambers of
the digestive tract and start with colorectal cancers. Off we go!
What Campbell overlooks about colorectal
cancers and cholesterol
As I mentioned earlier, a little somethin’ called
“schistosomiasis” is a profoundly strong risk factor for developing colon cancer
and rectal cancer. In the China Study data, schistosomiasis correlates at +89***
with colorectal cancer mortality. Yes, 89—higher than any of the other 367
variables recorded.
This, ladies and gentlemen, is what we call a
positive correlation.
It just so happens that total cholesterol also
correlates with schistosomiasis infection, at a statistically significant rate
of +34*:
Basically, this means that areas with higher
cholesterol levels also had—for whatever reason—a higher incidence of
schistosomiasis infection. It’s hard to say for sure why this is, but it’s
likely that the high-cholesterol and high-schistosomiasis groups had a third
variable in common, such as infected drinking water or other source of
schistosomiasis exposure.
From this alone, it shouldn’t be too shocking that
higher cholesterol also correlates with higher rates of colorectal cancer
(+33*):
Clearly, we have three tangled-up variables to sort
through: total cholesterol, colorectal cancer rates, and schistosomiasis
infection. Is it really higher cholesterol that increases the risk of developing
colon and rectal cancers, or is the influence of schistosomiasis deceiving
us?
To figure this out, let’s look at what cholesterol
and colorectal cancer rates look like onlyin regions with zero
schistosomiasis infection. If cholesterol is a causative factor for colorectal
cancers, then cancer rates should still increase as total cholesterol rises.
The above graph showcases a correlation of +13. Still
positive, but not statistically significant, and a major downgrade from the
original correlation of +33*. It does seem schistosomiasis inflates the
correlation between cholesterol and colorectal cancers—something Campbell never
takes into account. Is blood cholesterol still a risk factor? It’s possible, but
we would need more data to know whether the +13 correlation persists or whether
there are additional confounding variables at work. For instance, beer intake is
another factor correlating significantly with both total cholesterol (+32*) and
colon cancer (+40**). If we remove the three counties that drink the most beer
from of the data set above, the correlation between cholesterol and and
colorectal cancer drops to -9.
See how tricky the interplay of variables can be?
What Campbell overlooks about leukemia and
cholesterol
Next in our lineup of “Western diseases” is leukemia,
which has a statistically significant correlation of +26* with total
cholesterol. (Although the implication here is that animal product consumption
raises leukemia risk, it should be noted that animal protein intake itself has a
correlation of -5 with leukemia, whereas plant protein actually has a
correlation of +15 with this disease. But let’s humor this claim anyway by
looking solely at the role of blood cholesterol.)
If you’ll recall from the post on fish
and disease in the China Study, leukemia correlates very strongly with
working in industry (+53**) and inversely with working in agriculture (-53**).
Although it’s possible the cause is nutritional, it’s also quite likely that an
occupational hazard is to blame—such as benzene exposure, which is a major and
well-known cause of leukemia in Chinese factory and refinery workers.
Lo and behold, cholesterol also correlates strongly
with working in industry (+45**) and inversely with working in agriculture
(-46**). If an industry-related risk factor raises leukemia rates, it could very
well appear as a false correlation with cholesterol. How can we tell if this is
the case?
Let’s try looking at the correlation between leukemia
and cholesterol only in counties where few members of the population
were employed in industry. If cholesterol itself heightens leukemia risk, our
positive trend should still be in place. In the China Study data set, the range
for percent of the population working in industry is 1.1% to 41.3%, so let’s
try looking at the counties where the value is under 10%:
For the low-industry counties, the correlation
between leukemia and total cholesterol is close to neutral—a mere +4. As you can
see, this is hardly a damning trend. And in case you’re wondering if higher
cholesterol could possibly spur the rates of leukemia in folks who are already
at risk, this isn’t the case either: Using only counties that had 20%
or more of the population working in industry, presumably the folks who
had the most exposure to chemicals like benzene, the correlation between
cholesterol and leukemia is a slightly protective -3.
What Campbell overlooks about liver cancer
and cholesterol
I may not be vegan, but that doesn’t mean I like
beating dead horses. Instead of rehashing the earlier analysis of liver cancer
under Campbell Claim #3, I’ll just repeat that cholesterol
does not have a significant correlation with liver cancer when you
divide the data set into separate groups: areas with high hepatitis B rates an
areas with low hepatitis B rates.
From page 104 of his book:
Liver cancer rates are very
high in rural China, exceptionally high in some areas. Why was this? The primary
culprit seemed to be chronic infection with hepatitis B virus (HBV).
…
… But there’s more. In
addition to the [hepatitis B] virus being a cause of liver cancer in China, it
seems that diet also plays a key role. How do we know? The blood cholesterol
levels provided the main clue. Liver cancer is strongly associated with
increasing blood cholesterol, and we already know that animal-based foods are
responsible for increases in cholesterol.
Campbell connects some of the dots, but misses a very
important one. Indeed, hepatitis B associates strongly with liver cancer.
Indeed, cholesterol associates with liver cancer. But what he doesn’t mention is
that cholesterol also associates with hepatitis B infection.In other
words, the groups with higher cholesterol are already at greater risk of liver
cancer than groups with lower cholesterol—but it’s not because of diet.
In addition to greater rates of hepatitis B
infection, higher-cholesterol areas had additional risk factors for liver
cancer, such beer consumption, which also inflated the trend. Despite Campbell’s
claims, cholesterol itself does not appear to significantly heighten
cancer rates in at-risk populations.
Given Campbell’s casein research and earlier
observations about the animal-protein consuming children in the Philippines
getting more liver cancer, I wonder if Campbell approached the China Study
already expecting a particular outcome. In a massive data set with 8,000
statistically significant correlations, even a smidgen of confirmation bias can
cause someone to find a trend that isn’t truly there.
An example of bias in “The China
Study”
Body weight, associated with
animal protein intake, was associated with more cancer and more coronary heart
disease. It seems that being bigger, and presumably better, comes with very high
costs. (Page 102)
Consuming more protein was
associated with greater body size. … However, this effect was primarily
attributed to plant protein, because it makes up 90% of the total
Chinese protein intake. (Page 103)
Let’s read between the lines. Here
we have Campbell claiming two things, a few paragraphs apart: One, that body
weight is associated with more cancer and heart disease, and two, that body size
in China is linked not only with a greater intake of animal protein, but also
with a greater intake of plant protein. In fact, the link between body size is
stronger with plant protein than with animal protein.
Yet notice how Campbell only implicates
animal protein in the association between body weight, cancer, and heart
disease. If he were to describe the data without bias, Campbell’s first
statement would be this:
Body weight, associated with
animal protein intake and plant protein intake, was associated
with more cancer and more coronary heart disease.
Maybe his editor just overlooked that omission, eh?
Right afterward, Campbell notes:
But the good news is this:
Greater plant protein intake was closely linked to greater height and body
weight. Body growth is linked to protein in general and both animal and
plant proteins are effective! (Page 102)
Wait a minute. This is good news? Didn’t Campbell
just say being bigger “comes with very high costs” and that it’s associated with
“more cancer and coronary heart disease?” Why is body size a bad thing when it’s
associated with animal protein, but a good thing when it’s associated with plant
protein?
Does less animal foods equal better
health?
People who ate the most
animal-based foods got the most chronic disease. Even relatively small intakes
of animal-based food were associated with adverse effects. People who ate the
most plant-based foods were the healthiest and tended to avoid chronic
disease.
This oft-repeated quote from “The China Study” is
compelling, but is it true? Based on the data above, it seems like an unlikely
conclusion—but let’s try once more to see if it could be valid.
As an illustrative experiment, let’s look at the top
five Chinese counties with the lowestanimal protein consumption
and compare them against the top five counties with
thehighest animal protein consumption. A data set of 10 won’t
yield any confident conclusions, of course, and I won’t treat this as
representative of the collective body of China Study data. But since animal
protein consumption among the studied counties ranged from 0 grams* to almost
135 grams per day, we should see a stark contrast between the nearly-vegan
regions and the ones eating considerably more animal foods. That is, assuming
it’s true that “even relatively small intakes of animal-based food” yield
disease.
*The county averaging zero grams per day wasn’t
completely vegan, but the yearly consumption of animal foods was low enough so
that the daily average appeared less than 0.01 grams.
Here are the counties I’ll be using. The first five
are our near-vegans; the second five are our highest animal product consumers.
From both groups, I had to exclude a top-five county due to missing data for
most mortality variables (illegible documentation, according to the authors of
“Diet, Life-style and Mortality in China”) and replaced it with a sixth county
where animal protein consumption matched within a few hundredths of a gram.
Below are the names of each county, as well as values
for their daily animal protein intake, the percentage of their total caloric
intake coming from fat, and their daily intake of fiber (in case the latter two
variables are also of interest).
To give you a visual idea of these quantities, 135
grams of animal protein is the equivalent of 22 medium eggs per day, 24 grams of
animal protein is the equivalent of four medium eggs per day, 12 grams is two
eggs, and 9 grams is one and a half eggs. Obviously, that’s quite a wide range
even among the top consumers of animal foods, so the highest animal-food-eating
counties (Tuoli and XIanghuang qi) may be the most important to study in
contrast with the near-vegan counties.
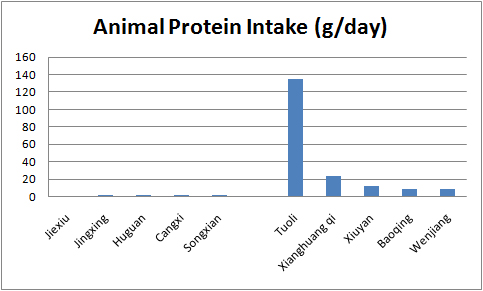
Animal protein intake by county:
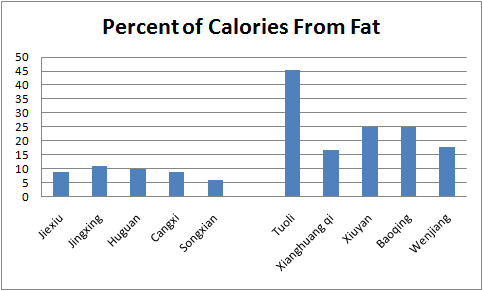
For reference, some other diet variables:
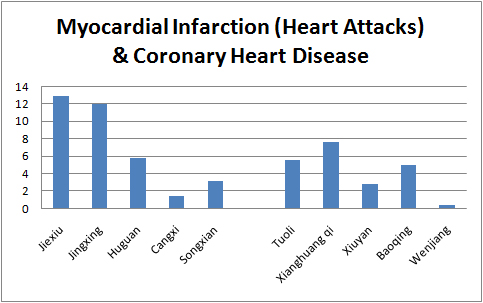
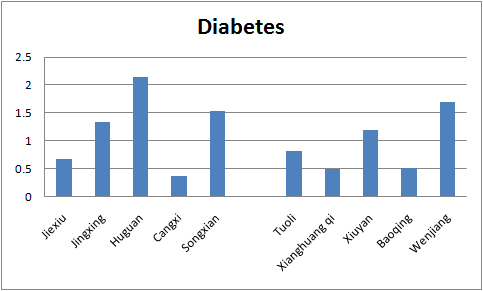
And now, mortality rates for important variables (as
per 1000 people). I’ll save you my commentary and just show you the graphs,
which should speak for themselves. Remember, the five left-most bars (Jiexiu
through Songxian) on each graph are the near-vegan counties, and the five
right-most bars (Tuoli through Wenjiang) are the highest consumers of animal
products.
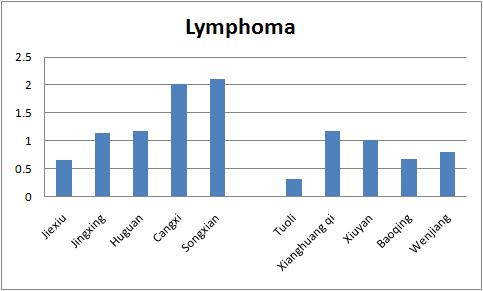
As you can see, the mortality rates for both groups
(near-vegan and higher-animal-foods) are quite similar, with the animal food
group coming out more favorably in some cases (death from all cancers,
myocardial infarction, brain and neurological diseases, lymphoma, cervix
cancer). This little comparison might not carry a lot of scientific clout due to
its small sample size, but it does blatantly undermine Campbell’s
assessment:
People who ate the most
animal-based foods got the most chronic disease … People who ate the most
plant-based foods were the healthiest and tended to avoid chronic
disease.
Sins of omission
Perhaps more troubling than the distorted facts in
“The China Study” are the details Campbell leaves out.
Why does Campbell indict animal foods in
cardiovascular disease (correlation of +1 for animal protein and -11 for fish
protein), yet fail to mention that wheat flour has a correlation of +67 with
heart attacks and coronary heart disease, and plant protein correlates at +25
with these conditions?
Speaking of wheat, why doesn’t Campbell also note the
astronomical correlations wheat flour has with various diseases: +46 with cervix
cancer, +54 with hypertensive heart disease, +47 with stroke, +41 with diseases
of the blood and blood-forming organs, and the aforementioned +67 with
myocardial infarction and coronary heart disease? (None of these correlations
appear to be tangled with any risk-heightening variables, either.)
Why does Campbell overlook the unique
Tuoli peoples documented in the China Study, who eat twice as much animal
protein as the average American (including two pounds of casein-filled dairy per
day)—yet don’t exhibit higher rates of any diseases Campbell ascribes
to animal foods?
Why does Campbell point out the relationship between
cholesterol and colorectal cancer (+33) but not mention the much higher
relationship between sea vegetables and colorectal cancer (+76)? (For any
researcher, this alone should be a red flag to look for an underlying variable
creating misleading correlations, which—in this case—happens to be
schistosomiasis infection.)
Why does Campbell fail to mention that plant protein
intake correlates positively with many of the “Western diseases” he blames
cholesterol for—including +19 for colorectal cancers, +12 for cervix cancer, +15
for leukemia, +25 for myocardial infarction and coronary heart disease, +12 for
diabetes, +1 for breast cancer, and +10 for stomach cancer?
Of course, these questions are largely rhetorical.
Only a small segment of “The China Study” even discusses the China Study, and
Campbell set out to write a publicly accessible book—not an exhaustive
discussion of every correlation his research team uncovered. However, it does
seem Campbell overlooked or ignored significant points when discerning the
overriding nutritional themes in the China Project data.
What about casein?
Along with trends gleaned from the China Project,
Campbell recounts the startling connection he found between casein (a milk
protein) and cancer in his research with lab rats. In his own words, casein
“proved to be so powerful in its effect that we could turn on and turn off
cancer growth simply by changing the level consumed” (page 5 of “The China
Study”). Protein from wheat and soy did not have this effect.
This finding is no doubt fascinating. If nothing
else, it suggests a strong need for more research regarding the safety of casein
supplementation in humans, especially among bodybuilders, athletes, and others
who use isolated casein for muscle recovery. Unfortunately, Campbell
extrapolates this research beyond its logical scope: He concludes that all forms
of animal protein have similar cancer-promoting properties in humans, and we’re
therefore better off as vegans. This claim rests on several unproven
assumptions:
- The casein-cancer mechanism behaves the same way in humans as in lab rats.
- Casein promotes cancer not just when isolated, but also when occurring in its natural food form (in a matrix of other milk substances like whey, bioactive peptides, conjugated linoleic acid, minerals, and vitamins, some of which appear to have anti-cancer properties).
- There are no differences between casein and other types of animal protein that could impose different effects on cancer growth/tumorigenesis.
Campbell offers no convincing evidence that any of
the above are true. We do share some metabolic similarities with rats, so for
the sake of being able to entertain the possibility that #2 and #3 are valid,
let’s assume that the effect of casein on rats translates cleanly to humans.
How does Campbell justify generalizing the effects of
casein to all forms of animal protein? Much of it is based on a study he helped
conduct: “Effect of dietary protein quality on development of
aflatoxin B[1]-induced hepatic preneoplastic lesions,” published in the August
1989 edition of the Journal of the National Cancer Institute. In this study, he
and his research crew discovered that aflatoxin-exposed rats fed wheat gluten
exhibited less cancer growth than rats fed the same amount of casein. But get
this: When lysine (the limiting amino acid in wheat) was restored to make the
gluten a complete protein, the rats had just as much cancer occurrence as the
casein group. Jeepers!
Campbell thus deduced that it’s the
amino acid profile itself responsible for spurring cancer growth. Because most
forms of plant protein are low in one or more amino acids (called “limiting
amino acids”) and animal protein is complete, Campbell concluded that animal
protein, but not plant protein, must encourage cancer growth. Time to whip out
the veggie burgers!
Of course, this conclusion has some
gaping logical holes when applied to real life. Unless you consume nothing but
animal products, you’ll be ingesting a mixed ratio of amino acids by default,
since animal foods combined with plant foods still yield limiting amino acids.
The rats in Campbell’s research consumed casein as their only protein source,
the equivalent of someone eating zero plant protein for life. An unlikely
scenario, to be sure.
Moreover, certain combinations of
vegan foods (like grains and legumes) have complementary amino acid profiles,
restoring each other’s limiting amino acid and resulting in protein that’s
complete or nearly so. Would these food combinations also spur cancer growth?
How about folks who pop a daily lysine supplement after eating wheat bread? If
Campbell’s conclusions are correct, it would seem vegans could also be
subject to the cancer-promoting effects of complete protein, even when eschewing
all animal foods.
Also, it seems Campbell never
mentions an obvious implication of a casein-cancer connection in
humans: breast milk, which contains high levels of casein. Should women
stop breastfeeding to reduce their children’s exposure to casein? Did nature
really muck it up that much? Are children who are weaned later in life at
increased risk for cancer, due to a longer exposure time the casein in their
mothers’ milk? It does seem strange that casein, a substance universally
consumed by young mammals, is so hazardous for health—especially since it’s
designed for a time in life when the immune system is still fragile and
developing.
At any rate, Campbell’s theories about plant versus
animal protein and cancer are essentially speculation. Despite a single
experiment with restoring lysine to wheat gluten, he hasn’t actually offered
evidence that all animal protein behaves the same way as
casein.
But check this out. After delineating his discovery
of the link between casein and cancer, Campbell writes:
We initiated more studies
using several different nutrients, including fish protein,
dietary fats and the antioxidants known as cartenoids. A couple of excellent
graduate students of mine, Tom O’Conner and Youping He, measured the ability of
these nutrients to affect liver and pancreatic cancer. (Page 66)
So he did experiment with an animal protein
besides casein! Unfortunately, Campbell never mentions what the specific results
of this research were. In describing the studies he conducted with his grad
students, Campbell says only that a “pattern was beginning to emerge: nutrients
from animal-based foods increased tumor development while nutrients from
plant-based foods decreased tumor development.” (Page 66)
I don’t know about you, but I’d sure like to see the
actual data for some of this.
After a little searching, I found one of the
aforementioned experiments conducted by Campbell, his grad student Tom, and two
other researchers. It was published in the November 1985 issue of the Journal of
the National Cancer Institute: “Effect of dietary intake of fish oil and fish
protein on the development of L-azaserine-induced preneoplastic lesions in the
rat pancreas.”
(A preneoplastic lesion, by the way, is a fancy term for the growth that occurs before a
tumor.)
In this study, Campbell and his team studied three
groups of carcinogen-exposed rats: One fed casein plus corn oil, one fed fish
protein plus corn oil, and one fed fish protein plus fish oil (from a type of
high omega-3 fish called menhaden). All groups received a diet of about 20%
protein and 20% fat and ate the same amount of calories.
Providing background for the study, the authors note
that previous research has showed fish protein to have anti-cancer properties
(emphasis mine):
Gridley et al. [n15,n16]
reported on two studies in which intake of fish protein resulted in a
reduced tumor yield when compared to other protein sources. Spontaneous
mammary tumor development in C3H/HeJ mice was reduced. The incidence of herpes
virus type 2-transformed cell-induced tumors in mice was also reduced in animals
fed a fish protein diet.
Perhaps this should’ve tipped
Campbell off that not all sources of animal protein spur cancer growth like
casein does. For reference, the cited studies are “Modification of herpes 2-transformed cell-induced tumors in mice fed
different sources of protein, fat and carbohydrate” published in the
November-December 1982 issue of Cancer Letters, and “Modification of spontaneous mammary tumors in mice fed different
sources of protein, fat and carbohydrate” published in the June 1983 issue of
Cancer Letters.
So what were the results of
Campbell’s experiment? According to the study, both the
casein/corn oil and fish protein/corn oil groups had significant preneoplastic lesions. We don’t know
whether to blame this on the protein or the corn oil,
since—according to the researchers—“intake of corn oil has previously been shown to promote the
development of L-azaserine-induced preneoplastic lesions in rats.” However, the
group that ate fish protein plus fish oil exhibited something radically
different:
It is immediately apparent that menhaden oil had a dramatic
effect both on the development in the number and size of preneoplastic
lesions. The number of AACN per cubic centimeter and the mean diameter
and mean volume were significantly smaller in the F/F [fish protein and fish
oil] groupcompared to the F/C [fish protein and corn oil] group.
Furthermore, no carcinomas in situ were observed in the F/F
group, whereas the F/C group had an incidence of 3 per 16 with 6 total
carcinomas.
There’s some significant stuff here, so let’s break
this down point by point.
One: The cancer-inducing
properties of fish protein, if there are any to begin with, were neutralized by
the presence of fish oil. This means that even if all animal protein behaves
like casein under certain circumstances, its effect on cancer depends on what
other substances accompany it. Animal protein is therefore not a
universal cancer promoter; only a situational one, at best.
Two: What does “fish protein” plus “fish fat” start
to resemble? Whole fish. Campbell just demonstrated
that animal protein may, indeed, operate differently when consumed with its
natural synergistic components.
Since there wasn’t a rat group
eating casein plus fish oil, we don’t know what the effect of a dairy protein
plus fish fat would have been. However, it would be interesting to have more
studies looking at cancer growth in mice fed diets of casein plus milk fat. If
casein loses its cancer-promoting abilities under that circumstance, as fish
protein did with fish oil, then we’d have good reason to think the various
factions of whole animal products might reduce any cancer-promoting
properties a single component has in isolation.
And Campbell and his team conclude:
[A] 20% menhaden oil diet,
rich in omega 3 fatty acids, produced a significant decrease in the development
of both the size and number of preneoplastic lesions when compared to a 20% corn
oil diet rich in omega 6 fatty acids. This study provides evidence that
fish oils, rich in omega 3 fatty acids, may have potential as inhibitory agents
in cancer development.
Remember how Campbell said,
summarizing this research, that “nutrients from animal-based foods
increased tumor development while nutrients from plant-based foods decreased
tumor development”? Last I checked, fish oil ain’t no plant food.
Why does Campbell avoid mentioning anything
potentially positive about animal products in “The China Study,” including
evidence unearthed by his own research? For someone who has openly censured the
nutritional bias rampant in the scientific community, this seems a tad
hypocritical.
But back to casein and milk for a moment. It’s
interesting that the only dairy protein Campbell experimented with was casein,
since whey—the other major protein in milk products—repeatedly shows
cancer-protective and immunity-boosting effects, including when tested
side-by-side with casein. Just a sampling of the literature:
- Diets containing whey proteins or soy protein isolate protect against 7,12-dimethylbenz(a)anthracene-induced mammary tumors in female rats. ” When 100% of the casein-fed rats had at least one tumor, soy-fed rats had a lower tumor incidence (77%) in experiment B (P < 0.002), but not in experiment A (P < 0.12), and there were no differences in tumor multiplicity. Whey-fed rats had lower mammary tumor incidence (54-62%; P < 0.002) and multiplicity (P < 0.007) than casein-fed rats in both experiments. … Furthermore, whey appears to be at least twice as effective as soy in reducing both tumor incidence and multiplicity.” (So much for plant protein being more protective against cancer!)
- Developmental effects and health aspects of soy protein isolate, casein, and whey in male and female rats. We found that SPI [soy protein isolate] accelerated puberty in female rats (p < .05) and WPH [whey protein hydrolysate] delayed puberty in males and females, as compared with CAS (p < .05). … Female rats fed SPI or WHP or treated with genistein had reduced incidence of chemically induced mammary cancers (p < .05) compared to CAS controls, with WHP reducing tumor incidence by as much as 50%, findings that replicate previous results from our laboratory.
- Tp53-associated growth arrest and DNA damage repair gene expression is attenuated in mammary epithelial cells of rats fed whey proteins. “Results indicate that mammary glands of rats fed a WPH [whey protein hydrolysate] diet are more protected from endogenous DNA damage than are those of CAS [casein]-fed rats.”
- A role for milk proteins and their peptides in cancer prevention. “Animal models, usually for colon and mammary tumorigenesis, nearly always show that whey protein is superior to other dietary proteins for suppression of tumour development.”
- A bovine whey protein extract stimulates human neutrophils to generate bioactive IL-1Ra through a NF-kappaB- and MAPK-dependent mechanism. “Our data suggest that WPE [whey protein extract] … has immunomodulatory properties and the potential to increase host defenses.”
- Whey proteins in cancer prevention.
- Whey protein concentrate (WPC) and glutathione modulation in cancer treatment.
Given all this, it seems unlikely that casein’s
effects on cancer apply to other forms of milk protein—much less all animal
protein at large. Isn’t it possible (maybe even probable) that casein has
deleterious effects when isolated, but doesn’t exhibit cancer-spurring qualities
when consumed with the other components in milk? Could casein and whey work
synergistically, with the anti-cancer properties of whey neutralizing the
pro-cancer properties of casein?
I’ll let you be the judge.
In summary and conclusion…
Apart from his cherry-picked references for other
studies (some of which don’t back up the claims he cites them for), Campbell’s
strongest arguments against animal foods hinge heavily on:
- Associations between cholesterol and disease, and
- His discoveries regarding casein and cancer.
For #1, it seems Campbell never took the critical
step of accounting for other disease-causing variables that tend to cluster with
higher-cholesterol counties in the China Study—variables like schistosomiasis
infection, industrial work hazards, increased hepatitis B infection, and other
non-nutritional factors spurring chronic conditions. Areas with lower
cholesterol, by contrast, tended to have fewer non-dietary risk factors, giving
them an automatic advantage for preventing most cancers and heart disease. (The
health threats in the lower-cholesterol areas were more related to poor living
conditions, leading to greater rates of tuberculosis, pneumonia, intestinal
obstruction, and so forth.)
Even if the correlations with
cholesterol did remain after adjusting for these risk factors, it takes
a profound leap in logic to link animal products with disease by way of blood
cholesterol when the animal products themselves don’t correlate with those
diseases. If all three of these variables rose in unison, then hypotheses
about animal foods raising disease risk via cholesterol could be justified. Yet
the China Study data speaks for itself: Animal protein doesn’t correspond with
more disease, even in the highest animal food-eating counties—such as Tuoli,
whose citizens chow down on 134 grams of animal protein per day.
Nor is the link between animal food consumption and
cholesterol levels always as strong as Campbell implies. For instance, despite
eating such massive amounts of animal foods, Tuoli county had the same average
cholesterol level as the near-vegan Shanyang county, and a had a
slightly lower cholesterol than another near-vegan county called
Taixing. (Both Shanyang and Taixing consumed less than 1 gram of animal protein
per day, on average.) Clearly, the relationship between animal food consumption
and blood cholesterol isn’t always linear, and other factors play a role in
raising or lowering levels.
For #2, Campbell’s discoveries with casein and
cancer, his work is no doubt revelatory. I give him props for dedicating so much
of his life to a field of disease research that wasn’t always well-received by
the scientific community, and for pursuing so ardently the link between
nutrition and health. Unfortunately, Campbell projects the results of his
casein-cancer research onto all animal protein—a leap he does not justify with
evidence or even sound logic.
As ample literature indicates, other forms of animal
protein—particularly whey, another component of milk—may have strong anti-cancer
properties. Some studies have examined the effect of whey and casein,
side-by-side, on tumor growth and cancer, showing in nearly all cases that these
two proteins have dramatically different effects on tumorigenesis (with whey
being protective). A study Campbell helped conduct with one of his grad students
in the 1980s showed that the cancer-promoting abilities of fish protein depended
on what type of fat is consumed alongside it. The relationship between animal
protein and cancer is obviously complex, situationally dependent, and bound with
other substances found in animal foods—making it impossible extrapolate anything
universal from a link between isolated casein and cancer.
On page 106 of his book, Campbell makes a statement I
wholeheartedly agree with:
Everything in food works
together to create health or disease. The more we think that a single chemical
characterizes a whole food, the more we stray into idiocy.
It seems ironic that Campbell censures reductionism
in nutritional science, yet uses that very reductionism to condemn an entire
class of foods (animal products) based on the behavior of one substance in
isolation (casein).
In sum, “The China Study” is a compelling collection
of carefully chosen data. Unfortunately for both health seekers and the
scientific community, Campbell appears to exclude relevant information when it
indicts plant foods as causative of disease, or when it shows potential benefits
for animal products. This presents readers with a strongly misleading
interpretation of the original China Study data, as well as a slanted
perspective of nutritional research from other arenas (including some that
Campbell himself conducted).
In rebuttals to previous criticism on “The China
Study,” Campbell seems to use his curriculum vitae as reason his word should be
trusted above that of his critics. His education and experience is no doubt
impressive, but the “Trust me, I’m a scientist” argument is a profoundly weak
one. It doesn’t require a PhD to be a critical thinker, nor does a laundry list
of credentials prevent a person from falling victim to biased thinking.
Ultimately, I believe Campbell was influenced by his own expectations about
animal protein and disease, leading him to seek out specific correlations in the
China Study data (and elsewhere) to confirm his predictions.
It’s no surprise “The China Study” has been so widely
embraced within the vegan and vegetarian community: It says point-blank what any
vegan wants to hear—that there’s scientific rationale for avoiding all animal
foods. That even small amounts of animal protein are harmful. That an ethical
ideal can be completely wed with health. These are exciting things to hear for
anyone trying to justify a plant-only diet, and it’s for this reason I believe
“The China Study” has not received as much critical analysis as it deserves,
especially from some of the great thinkers in the vegetarian world. Hopefully
this critique has shed some light on the book’s problems and will lead others to
examine the data for themselves.

















Nenhum comentário:
Postar um comentário